|
We are about halfway through Lung Cancer Awareness Month and I would like to offer some information about a fantastic organization. If you are reading this, you likely know about this group. But, even if you do, I encourage you to sit back with your favorite beverage and take a few minutes to watch the video at the end of this post. When supporting any cause or charity with a financial gift, prudent questions are “Where does the money go?”, “How effective is the organization?”, “Is it worthy of my support?”, "What are they doing?", "What have they done?" I ask these questions myself before choosing to financially support any charitable cause. This video, narrated by their Senior Director of Patient Services and Programs, Danielle Hicks, does an excellent job of answering these questions for The Bonnie J. Addario Lung Cancer Foundation (ALCF). My family and I met the Addarios shortly after our mother died in 2007. We were immediately struck by their sincerity, warmth - and tenacity. But, we were also impressed by their team and how they were attacking the lung cancer problem with intelligence and professionalism. In 2010, The Joan Gaeta Lung Cancer Fund proudly became an affiliate of ALCF. And, since 2012, those of you in Georgia have been able to order Lung Cancer Awareness License Plates - a first in the United States. 85% of the annual tag fee goes to ALCF’s research institute. You can also donate directly to ALCF via this link. Please to watch the video and consider a donation during this important month. Thank you, Joseph A. Gaeta The Joan Gaeta Lung Cancer Fund
0 Comments
Please help us in our continuing effort..... Donate today. Mortality
Incidence
Survival
Causes and Costs
SOURCES
We cannot think of a better way to kick of Lung Cancer Awareness Month 2016 than with this excellent Q&A with a leader in the movement - and our friend - Bonnie Addario. Please read this inspirational and informative interview from Genentech: https://www.gene.com/stories/qa-bonnie-j-addario
This article originally appeared at PschologyToday.com on July 26th, 2016. How does the stigma surrounding lung cancer delay diagnosis?by Theodora Ross, M.D., PhD.  Earlier this year, I appeared on NPR’s Fresh Air to discuss my recent book, A Cancer in the Family. During the interview, the conversation turned to ways individuals can reduce their risk for cancer. To make a point, I compared acting on knowledge of one’s genetic risk to smoking: “If you stop smoking or you don’t smoke,” I said, “the chances are you won’t get lung cancer.” Not long after, I received an email from a stranger with a subject line referencing the interview. The sender was a 43-year-old woman from California named Lisa who, despite never smoking or living with smokers, had been diagnosed with advanced-stage lung cancer at age 41. “I have never smoked a single cigarette,” she wrote. “I have never lived or worked with smokers. I have no other *known* risk factors for lung cancer either.” She told me she emphasized the word “known” due to the fact that little research has been done on non-smoking related causes of lung cancer. “I realize,” Lisa continued, “that your reference to smoking and lung cancer was just an off-hand remark and not the main point of your interview. However, lung cancer receives the least research funding of all the major cancers and has one of the poorest survival rates, due in large part to the stigma that statements, even casual ones like yours, perpetuate.” I replied with a lengthy apology for generalizing without providing context. But Lisa’s words echoed. Just hours before I had received that email, a colleague and I had been lamenting that if we could eliminate all incidents of cancer caused by lifestyle choices (many due to smoking), we’d have far fewer cancer cases today. This would leave time to study cancers with unknown causes, which would lead to better and faster diagnoses. And it would help end the stigma surrounding patients like Lisa—a stigma that I had inadvertently perpetuated on a national radio program. The stigmas and stereotypes around lung cancer need to be erased In 1964, when the first US Surgeon General’s Report on the health consequences of Smoking was published, 45 percent of adults smoked cigarettes despite stacks of evidence indicating that cigarettes caused lung and many other cancers. The year before, smoking in America had reached an all-time high thanks in large part to mass-market advertising campaigns during the previous few decades that falsely promoted smoking as a glamorous, even healthful, activity. In 2014, fifty years after that first Surgeon General’s Report, smoking has been identified as a leading cause of twenty-two diseases. Heart disease, which kills more people in the United States each year than any other illness, is at the top of the list. Many other organs dysfunction as a result of cigarettes and of course several cancers other than lung cancer are linked to cigarette smoking. Despite this, lung cancer has been singled out as the “smoker’s disease,” when in fact, it is one of many smoker’s diseases. Unfortunately, this fact leads to a stigma surrounding lung cancer patients—non-smokers and smokers alike—since people assume they could have prevented their disease. For non-smokers like Lisa, this can be an especially surprising twist to an already difficult diagnosis, even though there are many other patients like her. Currently, approximately 20 percent of lung cancer diagnoses in America (about 16,000-24,000 per year) occur in people who have never used tobacco products, and that fraction is on the rise, especially as smoking becomes less popular. (At present, only 15 percent of Americans smoke.) Additionally, many of the remaining 80 percent of lung cancer diagnoses are in former smokers, those who quit years or even decades before their diagnosis. Unfortunately, though, the stigma persists, and it can lead to devastating, even deadly, consequences. The problem of delayed diagnosis A close cousin of the stigma is the stereotype, wherein people make assumptions about someone or something based on preconceived, often incorrect, notions about others like them. Consider Lisa’s scenario: In the Fall of 2013, when she was 40 years old, she went to her doctor reporting fatigue and a cough that wouldn’t go away. Lisa was a fitness instructor, had never smoked, and had eaten a healthy diet for decades. The doctor never considered lung cancer a possibility, and prescribed codeine cough syrup. When the cough did not abate, Lisa returned to the doctor, who then prescribed an albuterol inhaler and antibiotics. Still, the cough persisted, and Lisa even began coughing up small amounts of blood. The doctor upped the prescription to steroids, gave her an Advair inhaler and then prednisone. The cough continued, and while she was on a family vacation, Lisa worsened and went to the local ER for a chest x-ray. She was told she had pneumonia. At this point, a family doctor/friend advised her to visit a pulmonologist. The pulmonologist obtained a chest CT, and Lisa had lung biopsy the following week. In January 2014, after months of misdiagnosis, she was finally diagnosed with Stage IV lung cancer, which has a survival rate of less than 10 percent. The situation was so dire that Lisa was offered “palliative” chemotherapy less than 48 hours after her diagnosis. If Lisa had smoked, her doctor would have known she was high risk and therefore likely ordered a CT scan sooner. But because her medical history did not align with the common perception of who a lung cancer patient is, her diagnosis came late. If we can catch lung cancer early enough for surgery, then we can cure patients. Delayed diagnosis is injustice. Lisa also has a significant family history of cancer (three grandparents and another close relative were all diagnosed with various types) but has not yet received a complete genetic test for inherited cancer gene mutations (those with which patients are born and that are found in all cells of the body, not just the tumor) that may show she is at risk for additional cancers. Patients with lung cancer are rarely sent for a genetic analysis even when, as in Lisa’s case, a genetic test is warranted based on National Comprehensive Cancer Network guidelines. Although, in this case, a test would not change her diagnosis, it could at least provide some much-sought answers about why she developed the disease. Let’s break the stigma Stigmas and stereotypes are lazy. They result from jumping to conclusions based on biases instead of facts, and they lead us into one-track thinking that prevents us from seeing the whole picture. Meanwhile, they wreak havoc on the lives of those who’ve been stigmatized, isolating them from their peers and rendering them the victims of prejudicial forces beyond their control. After I received Lisa’s email, I thought of how, in 1939, my Uncle Jack changed our family name from Rosenblum to Ross in order to increase his chances of getting a job. By changing his name, he avoided the stigmas and stereotypes associated with Jewish people and allowed himself to be considered on an even playing field with all the other candidates. It was unfortunate that such a change was necessary, but he got the job. Lung cancer patients can’t make this choice, so it is up to the rest of us to change our way of thinking in regard to the disease. Hopefully, one day soon people will quit cigarettes once and for all, and smoking-induced lung cancers will be a thing of the past. In addition to preventing suffering, this would allow researchers to dedicate more attention to other causes of lung cancer. In the meantime, let’s combat damaging stigmas and stereotypes by dealing in facts and choosing our words with care. When we do, we not only increase empathy, we save lives. Note: Lisa Goldman, who contributed to this piece, writes about her journey with lung cancer at Every Breath I Take. 7/31/2016 World Lung Cancer Day (August 1st ) Commemorates, Celebrates, and Supports Those Impacted by Lung CancerRead Now
GLENVIEW, Ill. (July 29, 2016) – On World Lung Cancer Day on August 1, the American College of Chest Physicians (CHEST), alongside members of the Forum of International Respiratory Societies (FIRS) commemorates, celebrates and supports those impacted by lung cancer. FIRS joins the grassroots efforts of the lung cancer community to raise awareness about lung cancer and its global impact, creating an educational movement of understanding lung cancer risks as well as early treatment around the world.
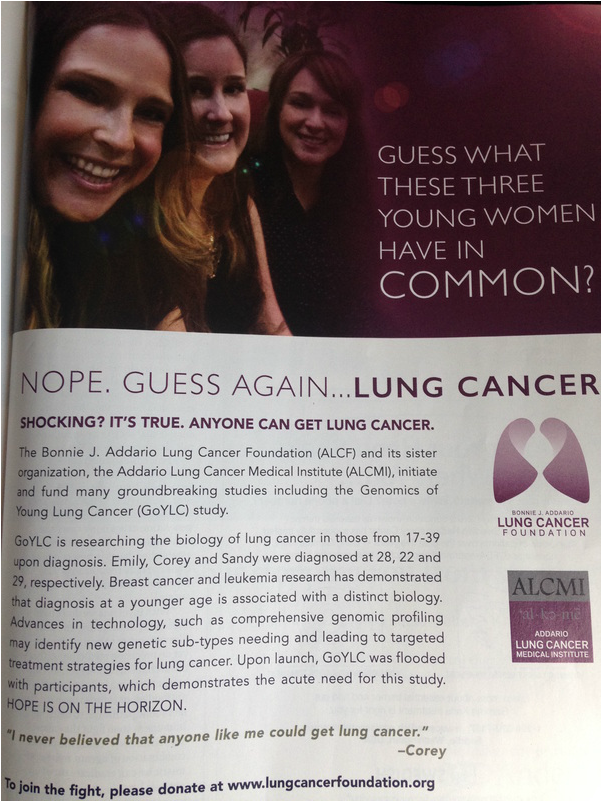
Lung cancer is the most common cancer worldwide, accounting for 1.8 million new cases in 2012, and is responsible for nearly one in five cancer deaths according to the World Health Organization. Lung cancer claims more lives yearly than breast, colon and prostate cancers combined. According to the American Cancer Society, an estimated 224,390 new cases of lung cancer are expected to be diagnosed in 2016, accounting for about 14% of all cancer diagnoses in the United States alone. World Lung Cancer Day 2016: Honor, Unite, Inspire highlights the many risk factors to be aware of in order to detect lung cancer at the earliest stage possible. While most understand that smoking is the single greatest risk factor for lung cancer, other lesser known risk factors include environment and genetics. Environmental exposure to radon, asbestos, arsenic, beryllium and uranium have all been linked to lung cancer. The risk of lung cancer also increases with a history of cancer in another part of the body, age, family history, radiation to the chest area and lung diseases like COPD. The initiative also aims to shed light on key symptoms and screening options. Symptoms include change in mucus, chest or back pain, coughing up blood and difficulty swallowing. Tests that may be used to diagnose lung cancer include chest X-rays, CT and PET scans, bronchoscopy and needle biopsies. If you are a current or former smoker and over age 55, you may be a candidate for a low- dose CT scan screening that can offer early detection of lung cancer, potentially at its earliest stages. “Treatment options for lung cancer have significantly advanced over the past few years and survival rates are increasing. We’re hopeful the World Lung Cancer Day efforts will help to continue to raise awareness of risks and increase early detection for the best possible outcomes,” said Dr. Gerard Silvestri, President-Elect of the American College of Chest Physicians. More than 70,000 global FIRS members have united in support of World Lung Cancer Day, including member organizations: CHEST, Asociación Latinoamericana del Thorax (ALAT), the American Thoracic Society, the Asian Pacific Society of Respirology, the European Respiratory Society, the International Union Against Tuberculosis and Lung Disease and the Pan African Thoracic Society. Patients, families and caregivers can download free educational resources and learn more about lung cancer, risk factors, screenings and treatment options by visiting http://www.chestnet.org/WLCD. About CHEST CHEST is the global leader in advancing best patient outcomes through innovative chest medicine education, clinical research and team-based care. Its mission is to champion the prevention, diagnosis and treatment of chest diseases through education, communication and research. CHEST serves as an essential connection to clinical knowledge and resources for its 19,000 members from around the world who provide patient care in pulmonary, critical care and sleep medicine. For more information, visit chestnet.org. About the Forum of International Respiratory Societies FIRS is an organization consisting of the world’s leading international respiratory societies working together to improve lung health globally: American Thoracic Society, CHEST, Asociación Latinoamericana De Tórax, Asian Pacific Society of Respirology, European Respiratory Society, International Union Against Tuberculosis and Lung Diseases and the Pan African Thoracic Society. The goal of FIRS is to unify and enhance efforts to improve lung health through the combined work of its more than 70,000 members globally. Contact: Kristi Bruno, [email protected] The Bonnie J. Addario Lung Cancer Foundation has a full-page ad in the June issue of Delta Air Lines' Sky Magazine! Way to go, guys! Thanks for spreading the word and helping to save lives!
5/10/2016 Patti LaBelle Encourages People to 'Share Their Voice ' in the Fight Against Lung CancerRead NowThis story and video were originally published at People.com by Christina Dugan on May 19th, 2016.
Patti LaBelle is kicking off National Women's Lung Health Week with a powerful message: share your voice.
The legendary gospel singer, 71, has joined the LUNG FORCE initiative through the American Lung Association. LaBelle, who has previously opened up to People about her personal connection to lung cancer, says that there is a lot of information that people aren't aware of. "I don't think people know that it's the No. 1 cancer killer of women, more so than breast cancer, colon cancer and pancreatic cancer combined," the gospel star said in December. "One woman dies every eight minutes in the United States of lung cancer. Bottom line: We all can do more to learn about lung cancer and contribute something to the initiative." In effort to spread the word, LaBelle and a church choir from Harlem have teamed up to create a touching video that encourages people to fight for a cure. "Making the video means so much to me because it's spreading awareness about a very important cause and I know that it is helping people," LaBelle tells People exclusively. In the video, LaBelle says, "I lost many important people in my life to lung cancer. It took two of my sisters in their early 40s and my choir director who helped me find my voice. Because they are no longer here to share their voices, I want to invite everyone to give 100 percent in the fight against lung cancer because 99 and a half won't do. There is hope. The more we come together, the more people will hear our message." She adds, "Thank you so much for sharing your voices. Let's do what we're put on this earth to do – let's all sing!" To donate, visit lungforce.org beginning Tuesday and enter for a chance to meet LaBelle and see her perform at an upcoming concert.
The state of Georgia provides its drivers the first – and only -specialty license plate in the country specifically dedicated to lung cancer awareness. Drivers in Georgia can alert fellow motorists that lung cancer matters!
The plates are available exclusively through The Joan Gaeta Lung Cancer Fund. Georgia drivers can learn more and begin the process of getting theirs at LungCancerLicensePlate.org.
The license plate is sponsored by The Joan Gaeta Lung Cancer Fund, a non-profit based in Atlanta that raises awareness and research funds for the number one cancer killer in the world.
 "My mother, Joan Gaeta, died of lung cancer after a three-and-a-half year battle," says Tina Pink, a VP of Fundraising for the Gaeta Fund. "She was most passionate about raising awareness and fighting the stigma of the disease. This plate is a big step in that direction. I know she would be very proud!" "My mother, Joan Gaeta, died of lung cancer after a three-and-a-half year battle," says Tina Pink, a VP of Fundraising for the Gaeta Fund. "She was most passionate about raising awareness and fighting the stigma of the disease. This plate is a big step in that direction. I know she would be very proud!"
Mrs. Pink's sister, Theresa Andretta, VP of Operations, concurs. "Lung cancer kills more people than the next five cancers combined! Yet, it receives the least amount of funding. We have no choice but to raise awareness and to fight the stigma. These plates are a great way to do that."
The $25 plate manufacturing fee, payable to The Joan GaetaLung Cancer Fund, helps them support ground-breaking research through the AddarioLung Cancer Medical Institute.
ABOUT THE JOAN GAETA LUNG CANCER FUND
The Joan Gaeta Lung Cancer Fund was created in the fall of 2007 as The Joan Gaeta Lung Cancer Foundation by her husband and children to raise awareness of the disease, to educate the public, and to be an advocate for research. They also strive to eliminate the stigma of lung cancer and to support survivors and their loved ones in their local community.
In July of 2010, they re-launched as The Joan Gaeta Lung Cancer Fund benefiting the Addario Lung Cancer Medical Institute. Their ultimate goal remains the same: “to eradicate lung cancer.†By partnering with one significant research initiative, they can make a much greater impact in wiping out lung cancer. http://www.forjoan.org
ABOUT THE ADDARIO LUNG CANCER MEDICAL INSTITUTE (ALCMI)
ALCMI was established in 2008 as a 501(c) (3) non-profit organization with the ultimate goal of significantly impacting survival by directly catalyzing and accelerating discovery of new and more effective treatment options for all lung cancer patients. Presently, ALCMI has 13 academic and community medical centers in the United States and Europe closely collaborating on cutting edge research initiatives. http://www.alcmi.net
ABOUT LUNG CANCER
-Even if you have never smoked, you can get lung cancer.
-60% of new cases are now diagnosed in non-smokers and former smokers.
-Lung cancer is the #1 cancer killer of both men and women.
-Every three minutes, someone is diagnosed with the disease.
-It kills more people each year than breast cancer, prostate cancer, colon cancer, liver cancer, melanoma, and kidney cancer combined.
-It surpassed breast cancer of the #1 killer of women in 1987.
-The five year survival rate for lung cancer is still only 15% - the same as it was nearly 40 years ago.
-Learn more at http://www.NobodyDeservesIt.com
Radon is a cancer-causing, radioactive gas. It is the leading cause of lung cancer among non-smokers. Radon is found all over the United States. Radon is a naturally occurring radioactive gas released in rock, soil, and water from the natural decay of uranium. While levels in outdoor air pose a relatively low threat to human health, radon can accumulate to dangerous levels inside buildings. You can’t see, smell, or taste it, but an elevated radon level in your home may be affecting the health of your family.
Exposure to radon is the second leading cause of lung cancer in the United States and the number one cause among non-smokers. The U.S. Environmental Protection Agency estimates that radon causes more than 20,000 lung cancer deaths in the country each year. Only smoking causes more lung cancer deaths. If you smoke and your home has radon, your risk of lung cancer can be higher. Radon has been found in elevated levels in homes in every state. No area of the country is free from risk. Indeed, two homes right next to each other can have vastly different radon levels. Just because your neighbor’s house does not have an elevated level of radon does not mean that your house will have a low radon level. The only way to know if your home is under the EPA action level of 4 pCi/L is to test. High levels of radon in homes usually come from the surrounding soil. Radon gas enters through cracks and openings—such as doors, windows, and plumbing features—on the lower levels of your home. Hot spots include basements, first-floor rooms, and garages, but radon can be found anywhere in your house. You Should Test for RadonThe U.S. Surgeon General recommends that all homes in the U.S. be tested for radon. Testing your house for radon is easy to do. If your house has a radon problem, you can take steps to fix it to protect yourself and your family. You can find out if your home has an elevated radon level by conducting a simple test. It’s as easy as opening a package, placing a radon detector in a designated area, and, after a set number of days, sending the detector back to a lab for analysis. The lab will then inform you of your radon test results. Radon test kits are available at your local home improvement or hardware store, or in some cases from your state radon office. You can also order them from the National Safety Council (NSC) or radon testing companies. Another option is to hire a qualified tester to do a radon test for you. Contact your state radon office about obtaining a list of qualified testers. Information about testing your home for radon and finding a test kit is also available by calling 1-800-SOS-RADON. Radon is measured in picocuries per liter of air (pCi/L), a measurement of radioactivity. EPA and the Centers for Disease Control and Prevention recommend that homes with radon levels at 4 pCi/L or higher should be fixed. EPA also recommends that Americans consider fixing their homes for radon levels between 2 pCi/L and 4 pCi/L. Based on a national residential radon survey completed in 1991, the average indoor radon level is about 1.3 pCi/L in the United States. The average outdoor level is about 0.4 pCi/L. You Can Fix a Radon ProblemThe cost of making repairs to reduce the radon level depends on several factors, including how your home was built. Most homes can be fixed for about the same cost as other common home repairs, like painting or having a new hot water heater installed. The average cost for a contractor to mitigate radon levels in a home is about $1,200, although costs can range from $800 to approximately $2,500. Look in your local phone book or call your state radon office to locate radon mitigators in your area if you find an elevated radon level in your home. New Homes Can Be Built with Radon-Resistant FeaturesRadon-resistant construction methods can be effective in reducing radon entry. When used properly, these simple and cost-effective techniques can help reduce the accumulation of radon gas in homes. Every new home should be tested after occupancy, even if it was built using radon-resistant construction methods. If radon levels above EPA’s action level of 4 pCi/L are are detected, it is easier and less expensive to reduce radon levels in homes that have been built with radon-resistant construction techniques. Radon presents a serious health risk, but it can be controlled easily and cost-effectively. Take action today. Encourage your friends and family members to do the same! Learn more from the EPA at http://www.radonmonth.org. More questions about radon? You can call one of the National Safety Council's Hotlines:
|
Details
|




 RSS Feed
RSS Feed
