|
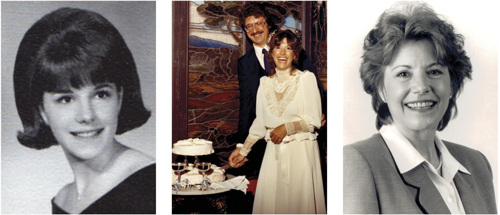
The following article was originally published in LSF Magazine: Summer 2012. Copyright 2012 Life Sciences Foundation. In late 2003, Bonnie J. Addario felt a shooting pain across her chest. Her physician suspected herniated disks, but prescribed therapies failed to alleviate her discomfort. Eventually, a CT (computed tomography) scan revealed a suspicious shadow on her left lung. Bonnie was informed by doctors that she had lung cancer, and that the tumor on her aortic arch was inoperable. She was fifty-seven years old. She went home. “I would never have believed it.” Before her diagnosis, Bonnie was an energetic wife, mother, and businessperson. She had never been sick, but she knew about unexpected reversals of fortune. When she tells her life story, she begins by saying: “If someone had told me this would be my path, I would never have believed it. Bonnie graduated from high school in 1965. “College wasn’t an option for me,” she says. “My parents were first-generation immigrants. My brothers were expected to go on. I was supposed to find a man.” Bonnie married and began raising a family. The union produced three children, but ended after twelve years with the family in dire financial straits. The young homemaker lost her house and car in the aftermath, and was forced into a series of menial jobs: “I did temp work for Kelly Girl. At night, I cleaned banks with my kids.” Suddenly, fortune smiled. Bonnie landed a permanent secretarial position at the Olympian Oil Company in South San Francisco. The company provided a range of services to gas and oil producers and marketers. Bonnie worked for the President and Chairman of the Board, performed well, and was rewarded with regular promotions. She displayed a knack for management: “I never went to business school. I figured it out along the way.” In little more than a decade, she became a retail manager, a supply distributor, an oil trader, and, finally, President of the company in 1997. Along the way, she had remarried. Life was good. Bonnie Addario’s success was unlikely, but her determination carried her through. Her untimely cancer diagnosis was a second potentially ruinous disruption in her life, and another test of will. “I sat in my kitchen and tried to relax,” she recalls. “I poured myself a glass of wine and opened the newspaper. My eyes went to a small article about a new cancer care partnership between the University of California, San Francisco [UCSF] and Sequoia Hospital, close to my home in Redwood City.” The partnership was spearheaded by UCSF thoracic surgeon Dr. David Jablons. Bonnie went to see him. He reviewed her case and offered a contrary opinion about surgery to remove the stage IIIB tumor – he believed that potential benefits outweighed the risks. “It will be a challenge,” he said, “but I’m up for it if you are.” Prior to the operation, Addario received radiation treatments five days a week, and chemotherapy every Friday, at Sequoia, in order to shrink the tumor and increase chances of a good outcome. The operation was a success. The surgeon removed the top left lobe of her lung, and part of her esophagus. The tumor was excised, although one of Bonnie’s vocal cords was paralyzed, and two major arteries in her heart were damaged and had to be repaired with grafts. After the surgery, Bonnie developed vascular necrosis, a side effect of steroids prescribed to moderate weight loss. The flow of blood to her bones was impeded. The bones became brittle, and she fractured her femur and hip as a result. She underwent two major surgeries to repair the breaks, and then, a few months later, was treated for a pulmonary embolism. When it was all over, Addario’s prognosis was upgraded. The ordeal left her physically depleted, but mentally charged. “My recovery was long and arduous,” she says. “I had plenty of time to think.” "I knew I had to EDUCATE people - patients, physicians, and the public - about lung cancer." Bonnie’s first instinct after her diagnosis had been to understand her condition and recruit expert medical counsel. Her search for information had been aggravating. Institutional support and education for lung cancer patients was virtually non-existent. The lack moved Addario to contemplate executive action in a new territory: “I knew I had to educate people – patients, physicians, and the public – about lung cancer.” The cancer that the NCI forgot Bonnie embarked on advanced studies in the biology, epidemiology, and politics of lung cancer. In conversation with other patients, she learned that the ‘standard of care’ is late-stage diagnosis, a dearth of treatment options, and poorly-coordinated medical services. She also learned that research on lung cancer is relatively neglected. In 1971, President Richard Nixon declared war on cancer. He signed the National Cancer Act into law, funneled a storm surge of federal dollars toward cancer research, and empowered the National Cancer Institute [NCI] to administer the funds. The legislation became a source of hope for cancer patients and their families, but lung cancer became the disease that NCI forgot. In the United States, lung cancer claims a life every three minutes. It takes twenty people per hour, 450 people per day. The disease kills more people than breast, prostate, colon, liver, skin, and kidney cancer combined, but funding for research on lung cancer lags behind all the rest. A mere 5% of the NCI’s research support budget is allotted to lung cancer projects. In 2001, the NCI’s Lung Cancer Progress Review Group, a panel of thirty expert clinicians, scientists, industry representatives, and patient advocates, reported that funding for studies of lung cancer was “far below the levels that characterize other common malignancies and far out of proportion to its massive public health impact.” The lopsided distribution has not been rectified. A comparison with breast cancer funding is telling. In 2008, lung cancer killed 161,840 Americans. NCI expenditures for lung cancer research amounted to $1,529 per lung cancer death. Breast cancer took 40,480 lives in 2008, but the NCI spent significantly more per breast cancer death: $14,145. Addario’s view of the situation is simple: “Funding should be distributed equitably.” A review of priorities in lung cancer research uncovers further issues. Sixty-two percent of NCI funds are earmarked for studies on prevention, causes, survivorship, and outcomes. Only 38% are dedicated to early detection, diagnosis, and treatment. Addario questions the wisdom of the apportionment. Many lung cancer patients receive stage IV diagnoses: “You have lung cancer. We’ll put you on Carboplatin and Taxol. Your hair will fall out. You’ll get sick and throw up. Then you’ll die.” Seventy-five percent of lung cancer patients die within eight to ten months of diagnosis. "The world still assumes, apparently, that only smokers get lung cancer. THAT IS NOT TRUE." Addario believes that NCI’s emphasis on prevention has to do with the fact that lung cancer is stigmatized as a “smoker’s disease.” Patients diagnosed with lung cancer are regularly asked if they smoked – it’s frequently the first thing they hear when someone learns of their condition. The question is an attempt to make sense of the world, to reduce the complexity of experience and discern order, but it’s simultaneously an attempt to assign blame. If lung cancer is the result of an individual’s decision to smoke, does it deserve as much attention as other common killers – breast cancer, prostate cancer, or colon cancer? Bonnie wants to set the record straight: “The world still assumes, apparently, that only smokers get lung cancer. That’s not true.” Some individuals are genetically predisposed to the disease, and environmental factors – atmospheric pollutants such as radon or the fine particulate matter found in smog, for example – contribute to the formation of lung tumors. Eighty percent of those diagnosed with lung cancer quit smoking decades earlier or never smoked at all. Addario objects to NCI’s funding priorities because studies of causation, prevention, and outcomes will not improve deficiencies in diagnosis and treatment – areas of pressing need that are not similarly deemphasized in, for example, breast cancer research. “The breast cancer movement has done a fabulous job,” Addario says. “The five-year survival rate for breast cancer is now above 90%. We want to achieve the same kind of results for lung cancer.” The five-year survival rate for lung cancer is 15.5%, and the figure hasn’t changed in 40 years. “That’s unacceptable,” Bonnie declares. “It can’t take another 40 years to make a difference. This needs to change!” Institutional impediments When Bonnie recovered her strength, Dr. Jablons asked her to join the UCSF Thoracic Oncology Cabinet, a multi-disciplinary advisory board established to help physicians with challenging or unusual cases, and to spearhead fundraising efforts for university departments involved in oncology research and care. Jablons spied an opportunity to add, in a single stroke, an experienced executive who understood organizational realities, and a cancer survivor who would infuse board deliberations with the patient’s perspective. Bonnie was introduced to Wells Whitney, the board chair. Whitney was also a patient of Jablons. Seven years earlier, he had been diagnosed with stage IV non-small cell lung cancer, and told that he had 10 to 12 months to live. Like Bonnie, his diagnosis spurred him to action. A scientist by training – he has a PhD in materials science from MIT — Whitney walked away from his job as Chief Scientist at Raychem, and immersed himself in scientific and medical literatures on lung cancer. He participated in the design of his own treatment regimen, and, against the odds, reduced the size of his tumor by 50%. The result qualified him to receive an operation usually reserved for early-stage patients. Bonnie recognized that she and Wells had much in common. Jablons’ intuition regarding Addario’s efficacy was soon confirmed. “My first assignment,” she recalls, “involved writing to my friends and asking them for money. I raised $75,000 in two weeks. The UCSF board probably thought, ‘We’ve got a live one here.’” But Bonnie didn’t want her efforts to begin and end with her checkbook. She wanted to do more than maintain the institution. In her view, doctors, scientists, and administrators were too comfortable with the status quo, and disinclined to consider radical reforms to established modes of research and treatment. Addario felt constrained by academia’s bureaucratic inertia. "That's unacceptable. It can't take another 40 years to make a difference. THIS NEEDS TO CHANGE!" “Informed patients live longer” Bonnie was eager to transform the ways in which lung cancer is understood and treated, and skeptical that universities could serve as catalysts of change. She decided to create a separate organization with a threefold mission – to provide patient support and advocacy, to educate and dispel misconceptions about the disease, and to heighten public awareness of the relative neglect of lung cancer research. With assistance from Whitney and Jablons, Bonnie established the Bonnie J. Addario Lung Cancer Foundation (BJALCF) in March of 2006. A few months later, the foundation made a public debut with a fundraising gala for lung cancer research in San Francisco. The evening drew a large crowd and raised an amount that was impressive (although “not nearly enough”). Bonnie was launched on her mission to fix a broken system. She was determined to improve the dismal statistics on lung cancer, one patient at a time. The BJALCF’s initial efforts were directed toward patient education and empowerment. The foundation’s first public awareness campaign urged patients to get CT imaging scans for early detection. The message (“CT Scan – think of it as a mammogram for your lungs”) was emblazoned in glowing pink and green on the sides of buses and highway billboards nationwide. The BJALCF soon refocused, however, and began organizing a diverse resource network through which patients and families could access information, support, and services. “We wanted to help people find their own best care,” Bonnie explains. “We connected them to experts, caregivers, and service providers at multiple sites. We focused on teaching people about what was available.” The goal was to help patients become their own advocates – just as Whitney and Addario had, with positive results. “Information is powerful,” says Bonnie. “Informed patients live longer. They just do.”
“If money were no object…” Patient empowerment was one piece of the puzzle. Addressing inequities in biomedical research was another. Bonnie saw that embedded attitudes and practices in the biomedical establishment needed to be perturbed and recast, and that the BJALCF needed to recruit thought leaders in lung cancer research to the cause. In order to make an impact on the conduct of laboratory and clinical research, the Foundation would need a bigger stage and the firm support of influential experts in science and medicine. Toward these ends, the BJALCF organized a meeting of world leaders in lung cancer research and care. On November 9, 2007 the best and the brightest in cancer research gathered in Genentech Hall on UCSF’s new Mission Bay campus for the first annual BJALCF Lung Cancer Summit. Wells Whitney served as master of ceremonies. Attendees included representatives from the NIH, Genentech, CancerCare, an oncology patient support organization, and Changing Our World, a philanthropy and fundraising consulting group. The keynote speaker for the two-day conference was Michael Milken, financier, philanthropist, cancer survivor, and founder of FasterCures, a self-described ‘action tank’ working to improve biomedical research. The all-star roster of physicians and cancer researchers on hand included Jablons, Dr. Pasi Jänne of the Dana Farber Cancer Institute, Dr. Mark G. Kris of the Memorial Sloan-Kettering Cancer Center, Dr. Fred Marcus of Sequoia Hospital and Dr. Harvey Pass of the NYU School of Medicine. As the researchers rose in succession to talk about their research, Bonnie realized that ingrained conference habits are hard to break. The summit was struggling with a terminal illness of its own: ‘death by powerpoint.’ Addario intervened, drew a curtain on the long string of self-congratulatory progress reports, and refocused the meeting. “We don’t want to know what you’re doing,” she said. “We want to know what you would change.” She challenged the attending scientists, physicians, lung cancer patients and survivors, venture capitalists, pharmaceutical industry executives, and government officials to answer one question: “If money were no object, what would you do to increase lung cancer survival rates?” Bonnie encouraged the group to momentarily forget the obstacles and imagine the possibilities. To be continued... Part II recounts how Bonnie J. Addario, in pursuit of improvements in lung cancer research and care, has pushed patient activism in new directions. She has formulated original ends for the BJALCF and devised innovative strategies for achieving them. Stay tuned.
1 Comment
7/29/2013 07:27:00 pm
I am really glad to know about such a great personality 'Bonnie J. Addario'. She is a role model for all the women and the society. She was brave enough to fought with her disease and overcome it. She is the symbol of women.
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
Details
|




 RSS Feed
RSS Feed
